Fear And Stress Living With Alzheimer’s And Other Dementias
Dementia is a general term that manifests from varied biological progressions that cause mutilation and/or loss of neurons and their processes within the brain.
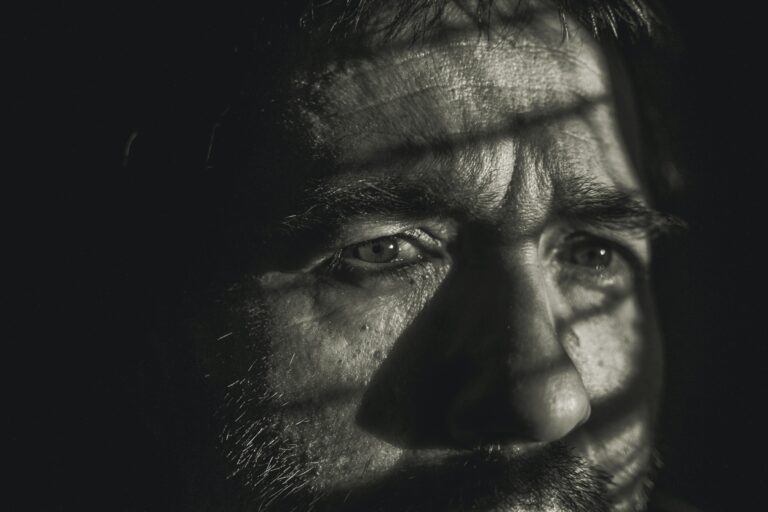
Alzheimer’s disease is a neurodegenerative disorder that leads to functional impairments of memory loss and cognitive decline and is the most common cause of dementia, accounting for 60-80% of dementia cases. Cognitive deterioration can cause stress and fear (Mehta, 2021 ). As many as 3 in 4 people with Alzheimer’s disease and Dementia may have some level of anxiety which can make them feel nervous, worried, or cause them to not want to be left alone or out of sight of their caregivers. Neuropsychiatric symptoms (NPS)are also associated with major adverse effects on daily function, quality of life, and reduced time to institutionalization. Aggression in dementia and Alzheimer’s patients also leads to job stress for nurses caring for these clients hence affecting the quality of care given. (Saina, 2021).
A number of studies indicate that Alzheimer’s patients exhibit neuropsychiatric symptoms including anxiety and depression that precede or present along with complaints of memory loss during the mild cognitive impairment (MCI) stage of the disease (Gillian Coughlan, 2019). Importantly, results from a recent meta-analysis indicated that anxiety increases the risk for progressing to dementia in patients with MCI (Lawrence S. Honig, Min Suk Kang, Nicole Schupf, & al, 2012). Additionally, individuals displaying sharp anxiety have a 48 % increased risk of developing Alzheimer’s disease(AD )and a faster rate of conversion from MCI to AD. However, the cause(s) of fear and stress in Alzheimer’s and dementia remains unclear, even though it has long been anticipated that anomalous metabolic oxidative reactions in the central nervous system (CNS) might have a pathological role. Thus, besides the pathological trademarks of the disease’s causes which include the accumulation of protein deposits in the brain as Ab plaques and as neurofibrillary tangles (NFT), AD brains exhibit constant evidence of reactive oxygen species (ROS)- and reactive nitrogen species (RNS)-mediated injury (Domenico Praticò, 2004) (Box 1). These reactive species are formed during standard metabolic reactions, are generally unbalanced from a chemical point of view, and are highly reactive. In some situations, the production of oxidant species can surpass the endogenous antioxidant capability to abolish them and an oxidative imbalance ensues. This occurrence results in cellular oxidative stress and consequent molecular oxidative impairment, which can translate into altered cellular functions and, as an ultimate result, cell death and ultimately lead to neuropsychic problems i.e. fear and stress in patients that are dealing with the disease of Alzheimer’s and dementia. (DomenicoPratic, 2008).
Further imperative modulators of oxidative stress, include reactive nitrogen species (RNS), including nitric oxide (NO) and peroxynitrite which can predominantly be extremely reactive with proteins, lipids, nucleic acid, and other molecules in further altering structure and/or functionalities leading to detrimental effects for the brain. (WEN-JUAN HUANG, 2016).
Living with Alzheimer’s or another dementia is not easy, but there is assistance for this journey. Don’t wait for others to offer support; be positive and reach out. The more sustenance you have, the better you’ll be able to deal with symptoms and continue to enrich your life.
- Stay connected with family and friends.
- Interact with your local Alzheimer’s Association.
- Seek out spiritual counsel(Coping with an Alzheimer’s or Dementia Diagnosis).
Recently, researchers at Weill Cornell Institute of Geriatric Psychiatry in New York studied the efficiency of a new home-delivered therapy called Problem Adaptation Therapy or PATH, in applicants with depression and dementia or mild cognitive impairment. In the PATH intercession, psychotherapists meet with the partakers in 12 weekly sittings to communicate to them how to unravel difficulties contributing to wretchedness, through a personalized approach often involving caregivers. The therapist and patient develop a plan, which contains circumventing undesirably charged circumstances and recognizing stimuli that activate encouraging emotions, such as scheduling pleasurable activities. (Stephanie Collier, 2020).


Superb post however I was wanting to know if you could write a litte more on this topic? I’d be very grateful if you could elaborate a little bit more.
Great post Thank you. I look forward to the continuation.
Thank you for great article. I look forward to the continuation.
As I website owner I believe the content material here is really good , appreciate it for your efforts.
I really like it when people come together and share opinions.
Great blog, stick with it!
Your article made me think about things I had never considered before. It’s always exciting to learn something new!
Your article helped me a lot, is there any more related content? Thanks!